04 Oct STRAIGHT TALK Vancouver researchers take issue with U.S. FDA’s alarmist memo on kratom
U.S. regulators appear to be moving against kratom, a plant originally from Southeast Asia that some people say has helped them with addictions to opioids like heroin by Travis Lupick on February 17th, 2018 at 8:00 AM11
2 of 2
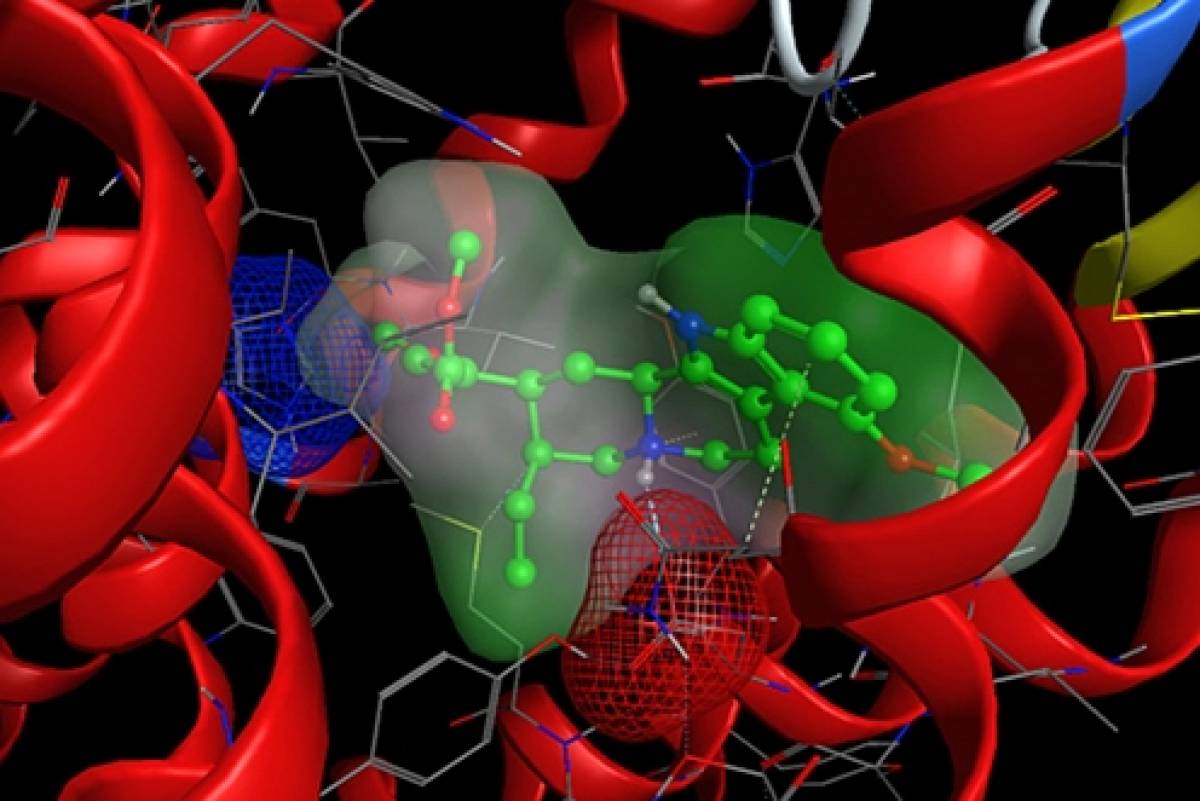
- The U.S. Food and Drug Administration recently used 3-D computer-modelling technology to predict how compounds that make up a plant called kratom interact with opioid receptors in the human brain.U.S. FOOD AND DRUG ADMINISTRATION
For a year or so now, Vancouver’s Downtown Eastside has buzzed with talk of a Southeast Asian plant called kratom.
The arrival of fentanyl has made an opioid addiction far riskier than ever before. And Mitragyna speciosa, as kratom is officially known, has been found to interact with the brain’s opioid receptors. What that means, early research has shown, is that it may help alleviate symptoms of opioid withdrawal and possibly function as a substitute that can help some people get off opioids entirely.
RELATED STORIES
- Natural kratom gains attention as a possible solution to opioid addiction, with science explaining how
- Preliminary count confirms more than 1,400 people in B.C. died after taking drugs in 2017
- How the worst overdose epidemic in Vancouver’s history left the Downtown Eastside to fend for itself
And so, in the Downtown Eastside, where there’s a concentration of people with addictions issues, kratom is being sold and shared as a substance that, for some people, works as an alternative to unknown substances that usually contain fentanyl.
But as the plant has attracted attention among people who use drugs, it’s also caught the interest of regulators.
On February 4, the U.S. Food and Drug Administration (FDA) issued a four-page statement on kratom that describes the plant as dangerous and without health benefits.
“We have been especially concerned about the use of kratom to treat opioid withdrawal symptoms, as there is no reliable evidence to support the use of kratom as a treatment for opioid use disorder and significant safety issues exist,” it reads.
“We now have 44 reported deaths associated with the use of kratom.”
The FDA’s memo sounds like there is obvious cause for significant concern. But two Vancouver researchers who have studied kratom for years told the Straight the document’s language is unjustifiably alarmist, based on questionable research, and contradicted by many academic papers on kratom.
“The FDA is creating, essentially, public hysteria,” Paula Brown, director of the B.C. Institute of Technology’s natural health and food products research group, said in a telephone interview. “I’m very skeptical that kratom could actually be attributed as a cause of death.”
Zachary Walsh, an associate professor in UBC’s department of psychology and co-director of the Centre for the Advancement of Psychological Science and Law, expressed the same skepticism for the FDA’s findings. He took issue with the evidence on which the FDA based the conclusions presented in its memo.
According to the document, the FDA used 3-D computer-modelling technology to simulate how the 25 most prevalent compounds that make up kratom interact with the human brain on a molecular level.
“In effect, PHASE [Public Health Assessment via Structural Evaluation] uses the molecular structure of a substance to predict its biological function in the body,” it reads. “The modelling platform can simulate how a substance will affect various receptors in the brain based on a product’s chemical structure and its similarity to controlled substances for which data are already available.”
Based on this method of computer modelling, the FDA says it found that kratom functions as an opioid. (“Opioid” is an umbrella term that includes heroin, fentanyl, morphine, and OxyContin, among other drugs).
“The model predicted that 22 (including mitragynine) of the 25 compounds in kratom bind to mu-opioid receptors,” the memo reads. “This model, together with previously available experimental data, confirmed that two of the top five most prevalent compounds (including mitragynine) are known to activate opioid receptors (‘opioid agonists’).
“The new data provides even stronger evidence of kratom compounds’ opioid properties,” it continues.

If kratom acts like an opioid, it must be dangerous, right? Brown and Walsh both told the Straight that’s not necessarily true.
“When you have one computer model interacting with another computer model, I’m reluctant to call it news,” Walsh said.
“It does seem to mimic some of the activities of opioids but it doesn’t cause respiratory depression,” he continued. “It does act on some of the same pathways [as opioids] and the subjective effects are somewhat similar but way weaker [than opioids].”
Brown said the same.
“Predicting compound activity by structural modelling and theoretical comparisons has been proven to be problematic and not terribly effective,” she explained. “This is a theoretical approach and cannot be considered empirical scientific evidence. We just can’t do a good job at predicting specific activity based on chemical structure.”
Both Vancouver researchers also took issue with the FDA’s dismissal of claims that kratom may assist some people addicted to opioids. Neither described kratom as a silver bullet for an opioid addiction. They were careful to stress that much more research is needed. But both pointed to studies that suggest that kratom may work for some people as an opioid substitute.
“Since the early 20th century in Southeast Asia, and increasingly in the U.S., kratom has been used as an opioid substitute for pain relief, opioid withdrawal, and maintenance of abstinence from prototypic dependence-producing opioids,” Brown said.
Walsh noted kratom has been used in countries such as Malaysia and Thailand for hundreds of years, and seemingly without significant problems such as widespread addiction or common overdose deaths.
“People do use it as an opioid substitute to help them cut down or reduce opioids,” he said. “We don’t yet know whether it’s effective in that way, although it’s difficult to imagine that we’d see that across different cultures and contexts if it wasn’t effective.”
A paper Walsh coauthored on kratom was published in the academic journal Drugs and Alcohol Dependence last October. The paper, a “systemic review” of existing scientific literature on kratom, presents findings very different from those of the FDA.
While the FDA’s memo states, “There is no evidence to indicate that kratom is safe or effective for any medical use,” Walsh’s paper states: “Findings indicate that kratom has potential as a harm reduction tool in the context of problematic opioid use.”
Walsh repeatedly emphasized more study is needed. But he argued that the dangers of using kratom appear substantially lower than the FDA describes them. And given the rate at which opioid addictions are killing people across North America, if kratom does work for some people as an opioid substitute, the plant’s potential benefits outweigh the known risks.
“I don’t think it’s going to be the answer to the opioid epidemic,” Walsh said. “But if it helps a little, that helps a lot.”Travis Lupick is a journalist based in Vancouver.

No Comments